Bronchiectasis resources for practitioners
Sometimes when you see COPD, chronic bronchitis, pneumonia, asthma or cystic fibrosis, you might also see bronchiectasis (BE)—a condition where the lungs’ airways are abnormally stretched and scarred resulting in mucus retention. It’s an under-diagnosed disease demanding action—and your attention.
Is it COPD—or BE?
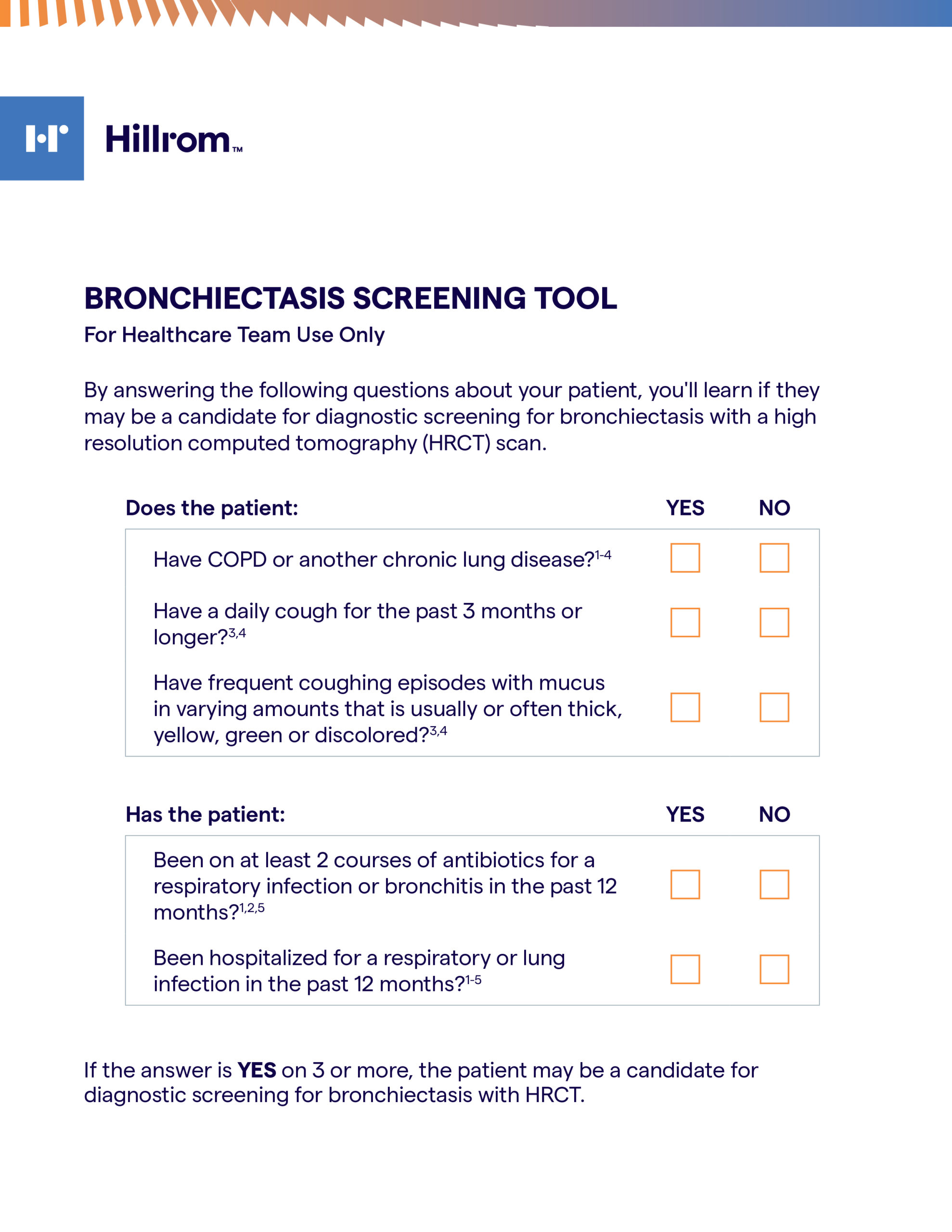
A CT scan can help determine a diagnosis of BE. Early diagnosis and intervention is the key to slowing the disease progression and helping your patients live better with BE.
Relatively common, especially as people age
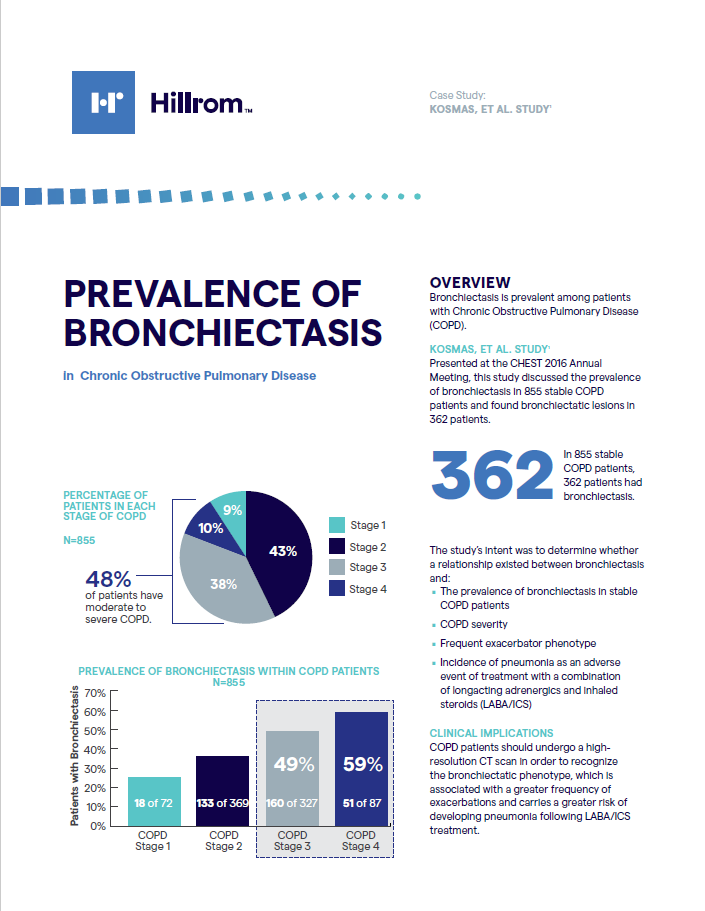
BE can frequently occur in parallel with more common forms of chronic lung disease.
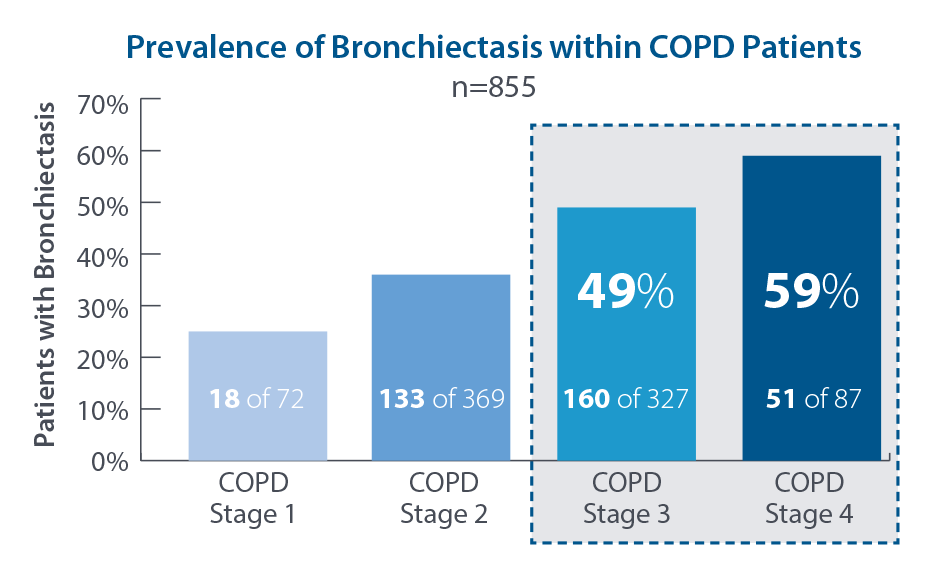
A recent study presented at CHEST 2016 Annual meeting demonstrated a prevalence of BE in moderate to severe COPD patients. 1
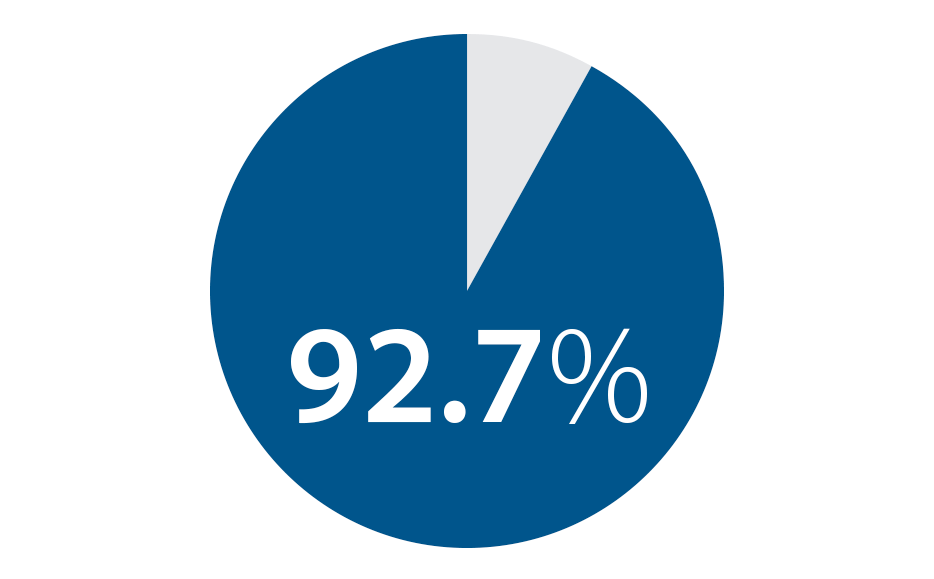
The same study showed that 92.7% of those COPD patients that had ≥ 2 exacerbations or at least 1 hospitalization per year had BE.1
Products for airway clearance
Although there is no cure for bronchiectasis (BE), early detection and treatment will allow patients to have a better quality of life and prevent further lung damage. Along with antibiotics and other appropriate medications, airway clearance therapies provide an effective, safe treatment. One category of airway clearance therapy is referred to as high frequency chest wall oscillation (HFCWO), also known as “vest therapy.”

How does high frequency chest wall oscillation (HFCWO) work?
HFCWO devices effectively treat all areas of your lungs by creating oscillating airflows that move mucus upward where it is easier to cough out. Keeping mucus from building up in your lungs helps to reduce the frequency of infection and hospitalizations, helps prevent further damage to your lungs and, best of all, helps you feel better. These airway clearance devices do not require special skills or techniques to administer quality airway clearance therapy—most patients are able to use them on their own. The system rapidly oscillates against the chest, gently compressing and releasing the chest wall, creating increased airflow within the lungs. This process thins and moves mucus toward the larger airways where it can be cleared by coughing or suctioning.
Connected in care
Some airway clearance devices include wireless transmission of therapy data that can be seen in a health portal. Some now include an easy-to-use patient app so patients can easily track their therapies as well. With both the patient and the healthcare team having access to the therapy information, it helps patients stay motivated with their therapy and allows the healthcare team to see usage information and trends over time.

Mobile Battery-Operated HFCWO
Another HFCWO device option is a mobile, battery-operated vest device that provides patients with HFCWO therapy without the need to be plugged into an electrical outlet. Like other HFCWO devices, this device rapidly oscillates against the chest wall to generate air pulses within the lung. The therapy generates airflow to help thin and move mucus from the airways, while allowing you to move about freely while doing your therapy.
Medicare Coverage Criteria for HFCWO
Bronchiectasis
Patient diagnosed with bronchiectasis:
Confirmed by a standard CT scan, which is characterized by:
a) Daily productive cough for at least six continuous months;
OR
b) Frequent (i.e. three or more in a year) exacerbations requiring antibiotic therapy;
AND
There must be well-documented failure of standard treatments to adequately mobilize retained secretions.
Examples of standard treatments:
- Manual Chest Percussion Therapy (CPT)
- Postural drainage
- Positive Expiratory Pressure (PEP) device
- Nebulized medication with mucolytic
Additional Resources
For more information on airway clearance therapies, visit Hillrom.com.
References
- Kosmas E, Dumitru S, Gkatzias S, et al. Bronchiectasis in patients with COPD: an irrelevant imaging finding or a clinically important phenotype? American College of Chest Physicians. Elsevier Inc., 2016. doi: http://dx.doi.org/10.1016/jchest.2016.08.994.
206967 rev 2 16-NOV-2020 ENG-US