Living with bronchiectasis
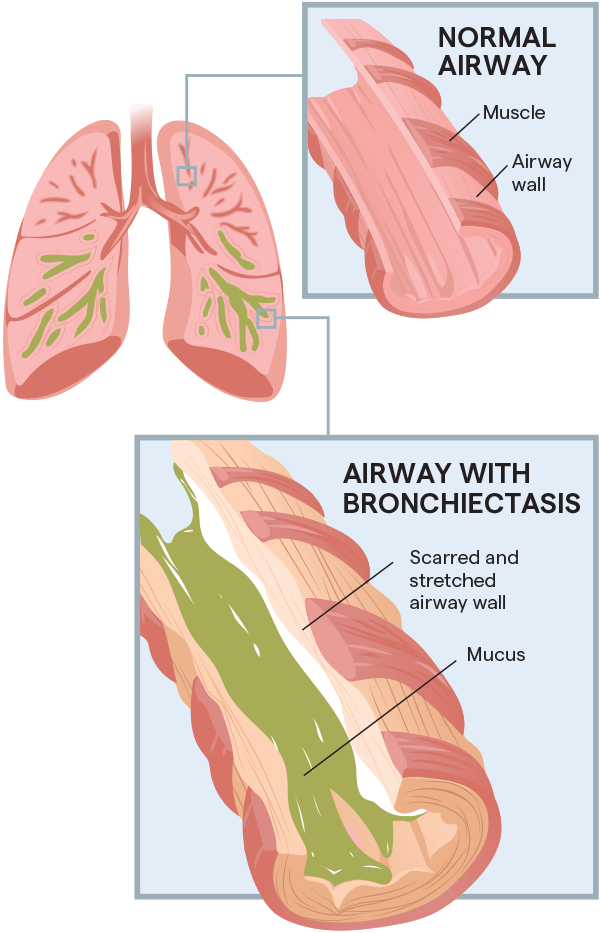
Bronchiectasis (brong-ke-EK-ta-sis) (BE) is a condition where the lungs’ airways are abnormally stretched and scarred, resulting in mucus buildup. Often it is caused by an infection or other condition that injures the walls of the airways or prevents mucus from being cleared.
With BE, lung inflammation and infection can become a repeating cycle:
- Airways slowly lose their ability to clear out mucus.
- The mucus builds up, and bacteria begin to grow.
- The patient can suffer from repeated, serious lung infections.

An under-diagnosed disease
It is estimated that more than 640,000 people in the U.S. are being treated for BE today—but experts believe many others go undiagnosed1. In a recent study, 44% of patients with moderate to severe COPD also had BE.2 Could you be one of them?

Common signs & symptoms
- Frequent cough that produces mucus
- Prescriptions for antibiotics for respiratory infections
- Hospitalization for respiratory infections
- History of lung disease

Living better with BE
While there is no cure, early detection and treatment can lead to a better quality of life and slow or prevent further lung damage. Along with medications, airway clearance therapies provide an effective, safe treatment.
If you have some of the symptoms associated with BE, you owe it to yourself to learn more. You can start by visiting this page and answering a few screening questions to determine if you may be candidate for a diagnostic screening.
Or, if you have already been diagnosed with BE, you can visit this Airway Clearance Therapy page to learn about treatment options.
References
1. Hillrom Market Research Report, 2018.
2. Kosmas E, Dumitru S, Gkatzias S, et al. Bronchiectasis in patients with COPD: an irrelevant imaging finding or a clinically important phenotype? American College of Chest Physicians. Elsevier Inc., 2016. doi: https://journal.chestnet.org/article/S0012-3692(16)57193-1/fulltext. Accessed 14 Aug 2020.
©2020 Hill-Rom Services PTE Ltd. ALL RIGHTS RESERVED.
206963 rev 2 18-AUG-2020 ENG – US

21 comments
Comments are closed.